Ifølge forskning præsenteret ved den Europæiske Kongress om Fedme afholdt i Wien den 23. maj, 2018, vil 22 % af verdens befolkning være fede i 2045, steget fra de 14 % den var sidste år. Et ud af otte mennesker steget fra et ud af elleve, vil have type 2 diabetes. I USA, har forskerne fundet at andelen af fede vil stige fra 39 % af befolkningen i 2017 til 55 % i 2045, og andelen diabetes vil stige fra 14 % til 18 %. I Storbritannien vil andelen øges fra 32 % til 48 % og hyppigheden af diabetes vil stiger fra 10,2 % til 12,6%.
Et hold forskere fik disse resulatater fra WHO's (World Health Organisation) database med data om befolkningerne fra alle verdens lande. De inddelte befokningerne i hvert land i aldersgrupper og yderligere efter body mass index (IBM) kategorierne, mens de så på tendenserne for at kunne lave fremskrivninger.
BMI, som er forholdet mellem højde og vægt, bruges til at inddele folk i lav og højrisikoskategorier i forhold til at udvikle hjertesygdomme, højt blodtryk, type 2 diabetes og visse typer kræft. En person med et BMI indeks på 25 eller mere anses som overvægtig og et indeks på 30 eller mere indikerer fedme. En sund BMI er i intervallet fra 18,5 til 24.9.
Modsat den almindelige opfattelse og selve definitionen, afslører BMI imidlertid ikke de mennesker, som har den største risiko for at udvikle hjertekarsygdomme og andre kroniske sygdomme, så som diabetes. Det er derfor lægerne har retningslinjer, som ignorerer BMI. I denne artikel vil vi lære om begrundelserne og implikationerne.
Kommentar: Delvist oversat af Sott.net fra The Age of Metabolic Syndrome - Inflammatory Fat Is Worse Than Obesity
Here Comes The Insulin Shock
After a "normal" meal, the body breaks down the constituent parts of food (fats, proteins and carbohydrates) into their smallest parts needed in order to absorb them. Carbohydrates get broken down into sugar in the digestive system which then gets absorbed into the bloodstream. Since high blood sugar is actually a dangerous state, the body takes care of all that sugar with the highest priority. It does this by releasing the hormone insulin.
Insulin is like the key that fits in the lock of the body's cells - it opens the doors for the sugar to get into the cells (and out of the bloodstream) in order to be burned. This process is referred to as glucose uptake. Meanwhile, the fat that was part of the meal needs to be put on hold until the sugar is dealt with. As well as letting sugar into the cells, insulin also turns off fat burning so that all the sugar can be burned first. Remember that the body needs to get that blood sugar back down quickly. As a result the body stores fat to be burned later. Unfortunately, given the high amount of carbohydrate in the average diet, with the constantly spiking insulin levels, the body doesn't get back to burning that fat any time soon.
If your carbohydrate intake is high, you'll end up storing both the fat and the carbohydrates in your body fat tissue thanks to the hormone insulin. When your diet is based on quickly absorbed sugars and carbohydrates (bread, pasta, rice, potatoes, etc.), the body slowly becomes resistant to the effects of insulin and needs more to do the same job of keeping your blood sugar even. High levels of insulin - "hyperinsulinemia" - leads to insulin resistance which in turn, leads to visceral fat accumulation which functions as a virtual factory for inflammatory signals.
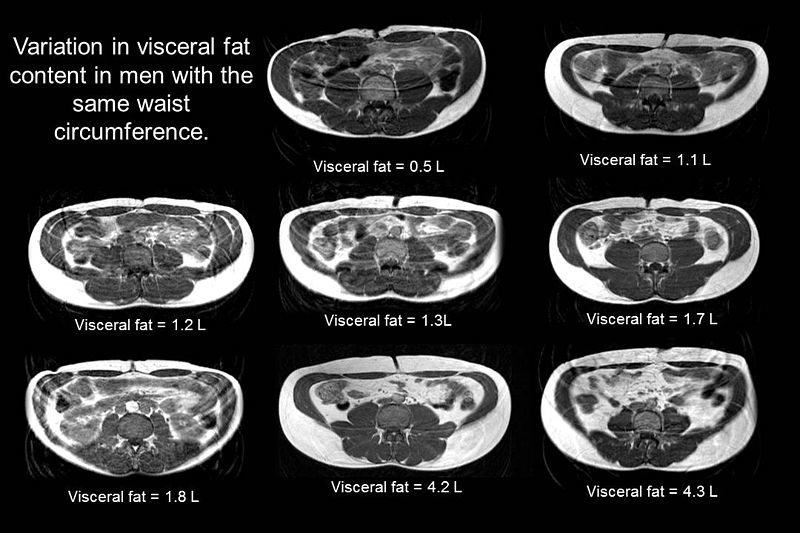
Deep abdominal fat encircling organs is correlated with insulin resistance and poor health. A person may have a normal BMI or be relatively thin, and still have deadly fat accumulated in visceral organs. An overweight person may have little to no fat accumulated in visceral organs, therefore at little risk for poor health. Most patients with cardiovascular disease that I saw in the operating room for heart surgery (coronary bypass) in Italy and Spain were not obese. Just once did we have to check the operating table limits for weight.
Since BMI alone is not enough to screen for inflammatory fat correlated with chronic disease, we need to take a closer look to one of the most prevalent forms of visceral fat.
Fatty Liver - Ducks Are Us
Fatty liver represents one manifestation of metabolic syndrome, a collection of symptoms often found together which features insulin resistance at its core but also includes increased abdominal circumference, high blood sugar, low good cholesterol (HDL), high blood pressure, and hypertriglyceridemia (high blood levels of triglycerides; fats). People on a low carbohydrate diet have better liver function compared to those on a high carbohydrate diet for weight loss, despite both groups losing weight equally (McCarthy and Rinella, 2012). In 30% to 50% of patient cases of fatty liver, diabetes is present (Wasserbach-York et al., 2009).
An expansion of central/visceral fat is associated with fatty liver and a state of heightened insulin resistance as well as increased oxidative damage (McCarthy and Rinella, 2012). They all go hand in hand. Fatty liver is an independent predictor of cardiovascular disease - a stronger predictor than peripheral fat mass (Schugar et al., 2012).
In a study involving 11,091 individuals, it was shown that fatty liver as diagnosed by ultrasound, strongly predicts the development of type 2 diabetes regardless of insulin concentration. That is, in a large population of relatively healthy individuals, identifying fatty liver by ultrasound accurately predicted the development of type 2 diabetes within five years (Sung and Kim, 2011).
Notice how foie gras (French for fatty liver and also a French delicacy) is made by force feeding large amounts of a wet mash of corn (not fat) to geese or ducks. Their livers balloon up to about 6-10 times their normal size, all packed full of fat. This serves as a good example of the fattening effects of carbs and how this promotes fatty deposition in the liver. The excess carbohydrates drive metabolic syndrome and it should come as no surprise that fructose is commercially derived from corn.

Fructose is also different from glucose in its ability to induce features of metabolic syndrome (insulin resistance, fatty liver, dyslipidemia, and intra-abdominal fat accumulation) both in humans and laboratory animals. The mechanism whereby fructose induces fatty liver appears to be independent of total energy intake (Lanaspa et al., 2012). So much for that low-calorie fructose meal!
Data from prospective and intervention studies clearly point to high fructose consumption, mainly in the form of sweetened beverages, as a risk factor for several metabolic diseases. In a short (2 week) dietary intervention study in fatty liver subjects, it was shown that carbohydrate restriction (<20 g/d) was significantly more effective in reducing liver fat content than the restriction of calories to 1200-1500 kcal/d (55% vs 28% liver fat reduction, respectively), despite the fact that both interventions similarly reduced body weight by about 4.3% (Rebollo et al., 2012).
But the problem doesn't end with sugar. While a diet high in carbohydrates leading to chronically elevated levels of blood sugar and insulin lies at the root of fatty liver, there are other culprits. Excess insulin triggered by a high carbohydrate diet strongly influences a pro-inflammatory response in the body, especially when coupled with excess omega-6 fatty acids from vegetable oil and hydrogenated oils.
People who get at least 25% of their daily calories from added sugars of any kind - fructose or other sugar sweeteners used by the food industry and consumers as ingredients in processed or prepared foods - are 3.1 times more likely to have low levels of so-called good cholesterol in their bloodstream than people who get less than 5% of their calories from added sweeteners. Additionally, those who consume more than 17.5% of their calories from the sugars - be it ordinary table sugar derived from sugar cane or sugar beets, high fructose corn syrup or any other caloric sweetener -are 20% to 30% more likely to have high levels of blood fats called triglycerides than people with the low-sugar diets (Welsh et al.,2010). The American Heart Association suggests no more than 5 percent of calories come from sugar. On a 2,000 calorie diet, that's 24 grams, or the equivalent of six teaspoons. A can of Coke has 39 grams of sugar; a regular size frozen yogurt has 40 grams.
Criteria for metabolic syndrome helps us determine if we have inflammatory fat, regardless if we're obese or not. It is a cluster of clinical signs that flags you for insulin resistance. Let's review again the criteria:
Notice how it doesn't include high total cholesterol nor high LDL cholesterol, only high triglycerides and low HDL. Metabolic syndrome is best correlated with high VLDL and dense LDL particles. If you are not familiarized with these terms, the following will help clarify.
The Unhealthy Cholesterol Panel
High cholesterol levels have long been singled out as a key player in cardiovascular disease and since saturated fat has been shown to increase cholesterol, it was recommended that saturated fat be avoided. But there is no correlation between high cholesterol levels and heart disease. The key is that the raw materials that we eat, the very basis of our diet, will later determine the quality of our cholesterol. Environmental and genetic factors also play an important role in our health and cholesterol. You see, within the context of a person's individuality, past and present history, cholesterol levels give us valuable information.
LDL (low density lipoprotein) has been incorrectly labeled as "bad cholesterol" and HDL (high density lipoprotein) as "good cholesterol". These terms are fictitious; in reality there is no such thing as "good" or "bad" cholesterol. It is important to understand that LDL and HDL are not cholesterol. They are types of lipoproteins which in themselves are spherical fat particles with water-soluble proteins around their exterior allowing them to travel our bloodstream unencumbered.
In short, they transport cholesterol to the tissues. HDL removes cholesterol from the tissues and returns it to the liver for disposal through the bile, where excess cholesterol is taken care of.
LDL transports cholesterol after production from the liver to the body's tissues.
Triglycerides are essentially the form that fat takes as it travels to the body's tissues through the bloodstream. And as it turns out, saturated fat doesn't increase triglycerides; on the contrary its levels go down on a low-carb diet (Hite, Berkowitz, & Berkowitz, 2011).
High triglyceride levels, a marker of poor health and an independent risk factor for heart disease, is unequivocally fueled by a high carb diet (including drinking too many fruit juices!). Triglycerides are high when there are problems in the body, particularly insulin resistance (which is a risk of diabetes) as well as inflammation (which is a risk of cardiovascular disease). High triglyceride levels are often seen with low HDL cholesterol levels, which is bad. HDL levels go down on a low-fat high carbohydrate diet - which is exactly what mainstream science recommend. No wonder doctors have such trouble seeing high levels of HDL in their practice! It is the triglyceride/HDL ratio that is a far more accurate predictor of cardiovascular disease than the so called "bad" cholesterol (Mclaughlin et al., 2005).
According to leading dietary researchers Dr. Jeff Volek and Stephen Phinney, M.D. (2011), the strongest correlation between a major dietary nutrient and blood levels of fat is with dietary carbohydrate, not with saturated fat intake. This may sound counter-intuitive; after all, surely eating more fat will lead to more of that fat ending up in the blood. But things in the body are rarely that cut and dried and such a simplistic view actually shows a complete lack of understanding of biochemistry. On average, it is actually the more carbohydrate that you eat that results in a higher content of evil fat in your blood. Once again, the high carb diet wreaks havoc.
Saturated fat doesn't decrease HDL cholesterol levels, in fact, it increases it (Volek, Sharman, & Forsythe, 2005). When you have high levels of HDL, you are less prone to infections and bowel cancer (Van Duijnhoven et al., 2011).
Saturated fat also contributes to the subcomponent of LDL cholesterol that is large, fluffy, and very hard to oxidize by environmental factors and inflammation in general. The image of saturated fat clogging up the arteries and producing heart attacks and strokes is now being recognized as the outdated medieval concept it really is, as researchers and clinicians finally admit what was known a long time ago - that it is really more about inflammation (Libby, Ridker,, & Maseri, 2002). Remember that a metabolism based on carbohydrates and burned polyunsaturated fatty acids (PUFAs) is more inflammatory than a metabolism based on animal fat, simply by the fact that carbs and PUFAs create more inflammatory free radicals when processed by the body.
Oxidized LDL particles constitute the other subcomponent of LDL cholesterol, and it's here where the only truth to the "cholesterol is bad" mantra holds some water. Oxidized LDL is essentially inflamed and tends to rise on a diet rich in inflammatory carbs, low in good fats, and high in burned polyunsaturated fats - pretty much the exact diet that has been recommended to us for over fifty years - lots of vegetable oils, "heart-healthy whole grains" and little to no saturated fat and cholesterol.
Truly healthy saturated fats, on the other hand, stabilize the omega-3s in our bodies and make it much less likely for anything, including LDL, to oxidize. The other factor that can oxidize LDL cholesterol is the amount of time of exposure to pro-oxidants. If it is exposed for a long time, LDL becomes denser (i.e. lipoprotein-a) and starts to oxidize.
It is the denser and smaller LDL cholesterol which is a marker of poor heart health and an indication of bad LDL receptors and physiological functioning. Small dense LDL particles are prone to oxidation and inflammation. It is this reason why atherosclerosis happens in arteries and not in the veins - the arterial blood, carrying blood from the lungs to the tissues, is rich in oxygen, a pro-oxidant, whereas venous blood is relatively poor in oxygen.
Another pro-oxidant factor is excess iron in the body, a problem typically seen in those who are genetically predisposed to absorb more iron from dietary sources. The excess iron oxidizes in your body and can literally rust your organs leading to diseases such as cancer, coronary artery disease, cirrhosis, arthritis and so forth.
The small LDL cholesterol particles can penetrate more easily the arterial wall leading to atherosclerosis and then a potential heart attack. Larger LDL particles have a harder time getting in.
The small, dense LDL cholesterol particles are much more vulnerable to glycation in your body. Glycation is the process where carbohydrates stick on to other molecules in the body, causing them to "caramelize". It ages and inflames the body. It is very damaging and it is enhanced by a diet rich in sugars (and all digestible carbs become sugars eventually!) and oxidized polyunsaturated fatty acids. And caramelized (glycated) LDL particles, lacking in their normal functionality, stay in circulation much longer, increasing their chance of being oxidized.
And as for triglycerides, in the words of cardiologist William Davis:
"Triglycerides reflect the level of very low-density lipoproteins, or VLDL, in the bloodstream. I therefore use triglycerides and VLDL as interchangeable terms. Triglycerides reflect a number of important metabolic phenomena, including blood sugar and insulin status (high triglycerides in type 2 diabetes, for instance), carbohydrate intake (via liver de novo lipogenesis, or the conversion of carbs to triglycerides), and volume of visceral fat that is made up of triglycerides that are continually released by fat cells into the bloodstream, then re-uptaken. (Although dietary fats are actually made of triglycerides, the contribution of dietary fat to fasting triglyceride levels is negligible, with some rare genetic exceptions. The relative contributions of carbs vs. fats in non-fasting, or postprandial, settings is an entirely different conversation.) High triglycerides/VLDL are also associated with having lots of small LDL particles, a potent cause for heart disease." (Davis, 2016, para. 8)In fact, in a study of almost 50,000 women followed for 8 years showed that restricting fat, which leads to reduced LDL cholesterol, had no effect on cardiovascular disease outcomes (heart attack, stroke, and overall mortality) (Howard et al., 2006). So why exactly are we trying so hard to keep LDL levels low? LDL is like the bogeyman of body metabolism - everyone is scared of it, mostly due to rumor and hearsay. Don't panic if your doctor tells you your LDL cholesterol is too high within the context of an anti-inflammatory diet restricted in carbs and high in good fats. As Stephen D. Phinney and Jeff S. Volek explain in The Art and Science of Low Carbohydrate Living (2011, p. 93-94):
"Less appreciated are the potential errors associated with low plasma triglycerides, a condition that is highly relevant when interpreting the LDL-C response to low carbohydrate diets since they often result in marked reductions in triglycerides.In other words, if you have low triglyceride levels, they are most likely overestimating your LDL cholesterol levels due to the fact that they use an equation to figure them out. The equation may be pretty accurate when looking at your average sugar-burner, but in a low-carb fat burner it becomes significantly flawed. In actuality, a low-carber's LDL levels could be much lower when measured by actual testing. These tests are rarely done. A low carb diet brings your triglyceride levels down, and that IS good. Low triglyceride levels are rarely if ever seen in the always recommended 'healthy' high-carb diet.
For example, a published case report describes a man with plasma triglycerides of 55 mg/dL who had an estimated LDL-C of 172 mg/dL using the traditional Friedewald equation. But when measured by two separate direct methods, his actual LDL-C proved to be 126 mg/dL.
In a formal study of 115 volunteers with plasma triglycerides less than 100 mg/dL, use of the Friedewald formula resulted in a statistically significant overestimation of LDL-C by an average of 12 mg/dL.
How does this play out if you are on a low carbohydrate diet? Let's assume that a low carbohydrate diet causes a reduction of triglycerides from 200 to 75 mg/dL with no change in total and HDL cholesterol. As a result, the calculated LDL-C from the Friedewald equation would necessarily increase from 100 to 125 mg/dL. How much of this 25% increase is real and how much artifact? That can only be determined by a direct assessment of LDL-C [LDL cholesterol], which most physicians do not bother to do."
Never in history have we seen such an incidence of diabetes and obesity as we see today. We have a figurative tsunami of diabetes cases around the world, a clear sign that something is very wrong with our diet and our dietary guidelines. Reverse the low fat recommendations and the health problems ease up for people at large. Diabetics and overweight people improve cholesterol levels, weight, and insulin levels with a low carb diet (Volek, Phinney, Kossoff, Eberstein, & Moore, 2011).
Current Dietary Guidelines Make Things Worse
We have seen how a normal BMI doesn't mean that you are healthy because it doesn't tell us if there is visceral fat.
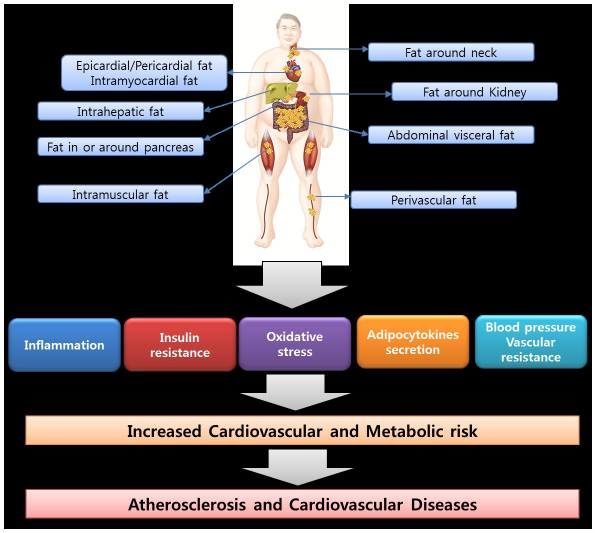
In mainstream circles, ectopic fat refers to the accumulation of fat in places where it shouldn't be: in organs, liver, muscles, heart, blood vessels, kidneys, neck and pancreas (Lim and Meigs, 2014). It acts as an "organ" which releases chemicals that promote insulin resistance, inflammation and coagulation factors.
Ectopic fat, which 'thin' people may have, increases inflammatory factors, oxidative stress, vascular resistance (high blood pressure), promoting any disease that has insulin resistance at its main component such as sleep apnea, diabetes, fatty liver, polycystic ovarian syndrome and Alzheimer's disease.
In muscles, triglyceride accumulation induces insulin resistance and cardiovascular disease. Muscle tissue is the main destination of fatty deposits and sugar loading via insulin. In kidneys, fat accumulation promotes high blood pressure or vascular resistance. In the pancreas, accumulated inflammatory fat impairs glucose metabolism and promotes inflammation and insulin resistance. In the neck, inflammatory fat promotes sleep apnea, insulin resistance and endothelial dysfunction. In the liver, fat accumulation induces insulin resistance, inflammation and oxidative stress. In the heart, inflammatory fat is related with calcification of the heart's vessels.
If you restrict animal fat in your diet, you end up increasing the intake of carbohydrates and vegetable oils. The research is so clear that mainstream doctors are beginning to receive more data related to this concept in their guidelines.
For instance, the PREDIMED study (Estruch et al., 2013) conducted in Spain revealed that by decreasing dietary fat, there were more cardiovascular events. People fared better when they used some olive oil or ate some fatty nuts.
The DiRECT study showed that those who restricted fat lost the least weight compared to those on a diet low in carbohydrates or those on a Mediterranean diet (Lean et al., 2018).
These are only two of the most recent cited papers in mainstream circles, but there are many others.
In addition, there is increasing awareness of vitamin D's role in sensitizing insulin and some are making connections between low levels of vitamin D and metabolic disease (Boteon-Schmitt et al., 2018).
I hope this helps to clarify the consequences of inflammatory fat within the body regardless of BMI and how the situation is critical considering that the increasing rates of obesity alone cannot be used as an indicator of ill health.
References
Boteon-Schmitt et al. Vitamin D deficiency is associated with metabolic syndrome in postmenopausal women. Maturitas, 2018; 107: 97 DOI: 10.1016/j.maturitas.2017.10.011
Davis, W. (2016, August 22). "Treat" cholesterol, exorcise the bogeyman. Retrieved from http://www.wheatbellyblog.com/2016/08/treat-cholesterol-exorcise-bogeyman/
Estruch et al. Primary Prevention of Cardiovascular Disease with a Mediterranean Diet. N Engl J Med 2013; 368:1279-1290
DOI: 10.1056/NEJMoa1200303
Hite, A. H., Berkowitz, V. G., & Berkowitz, K. (2011). Low-carbohydrate diet review. Nutrition in Clinical Practice, 26(3), 300-308. doi:10.1177/0884533611405791
Howard, B. V., Horn, L. V., Hsia, J., Manson, J. E., Stefanick, M. L., Wassertheil-Smoller, S., . . . Kotchen, J. M. (2006). Low-fat dietary pattern and risk of cardiovascular disease: The Women's Health Initiative Randomized Controlled Dietary Modification Trial. JAMA, 295(6), 655-666. doi:10.1001/jama.295.6.655
Lanaspa et al. Uric Acid Stimulates Fructokinase and Accelerates Fructose Metabolism in the Development of Fatty Liver. PLoS One. 2012; 7(10): e47948.
Lean et al. Primary care-led weight management for remission of type 2 diabetes (DiRECT): an open-label, cluster-randomised trial. The Lancet. Volume 391, No. 10120, p541-551, 10 February 2018
Libby, P., Ridker,, P. M., & Maseri, A. (2002). Inflammation and atherosclerosis. Circulation, 105(9), 1135-1143. doi:10.1161/hc0902.104353
Lim S, Meigs JB. Links between ectopic fat and vascular disease in humans. Arteriosclerosis, thrombosis, and vascular biology. 2014;34(9):1820-1826. doi:10.1161/ATVBAHA.114.303035.
McCarthy and Rinella. The role of diet and nutrient composition in nonalcoholic fatty liver disease. Journal of the Academy of Nutrition and Dietetics. 2012;112:401-409.
Mclaughlin, T., Reaven, G., Abbasi, F., Lamendola, C., Saad, M., Waters, D., . . . Krauss, R. M. (2005). Is there a simple way to identify insulin-resistant individuals at increased risk of cardiovascular disease? The American Journal of Cardiology, 96(3), 399-404. doi:10.1016/j.amjcard.2005.03.085
Rebollo et al. Way back for fructose and liver metabolism: bench side to molecular insights. World J Gastroenterol 2012 December 7; 18(45):6552-6559
Schugar et al. Low-carbohydrate ketogenic diets, glucose homeostasis, and nonalcoholic fatty liver disease. Curr Opin Clin Nutr Metab Care 2012, 15: 374-380.
K.C. Sung, S. H. Kim. Interrelationship between Fatty Liver and Insulin Resistance in the Development of Type 2 Diabetes. Journal of Clinical Endocrinology & Metabolism, 2011; DOI: 10.1210/jc.2010-2190
Van Duijnhoven, F. J., Bueno-De-Mesquita, H. B., Calligaro, M., Jenab, M., Pischon, T., Jansen, E. H., . . . Riboli, E. (2011). Blood lipid and lipoprotein concentrations and colorectal cancer risk in the European Prospective Investigation into Cancer and Nutrition. Gut, 60(8), 1094-1102. doi:10.1136/gut.2010.225011
Volek, J. S., Phinney, S. D., Kossoff, E., Eberstein, J. A., & Moore, J. (2011). The art and science of low carbohydrate living: An expert guide to making the life-saving benefits of carbohydrate restriction sustainable and enjoyable. Lexington, KY: Beyond Obesity.
Volek, J. S., Sharman, M. J., & Forsythe, C. E. (2005). Modification of lipoproteins by very low-carbohydrate diets. The Journal of Nutrition, 135(6), 1339-1342.
Wasserbach York et al. Nonalcoholic fatty liver disease and low-carbohydrate diets. Annu. Rev. Nutr. 2009 29:365-79
Welsh et al. Caloric Sweetener Consumption and Dyslipidemia Among US Adults. JAMA, April 21, 2010 - Vol 303, N. 15, 1490-1497.


Læserkommentarer
dig vores Nyhedsbrev